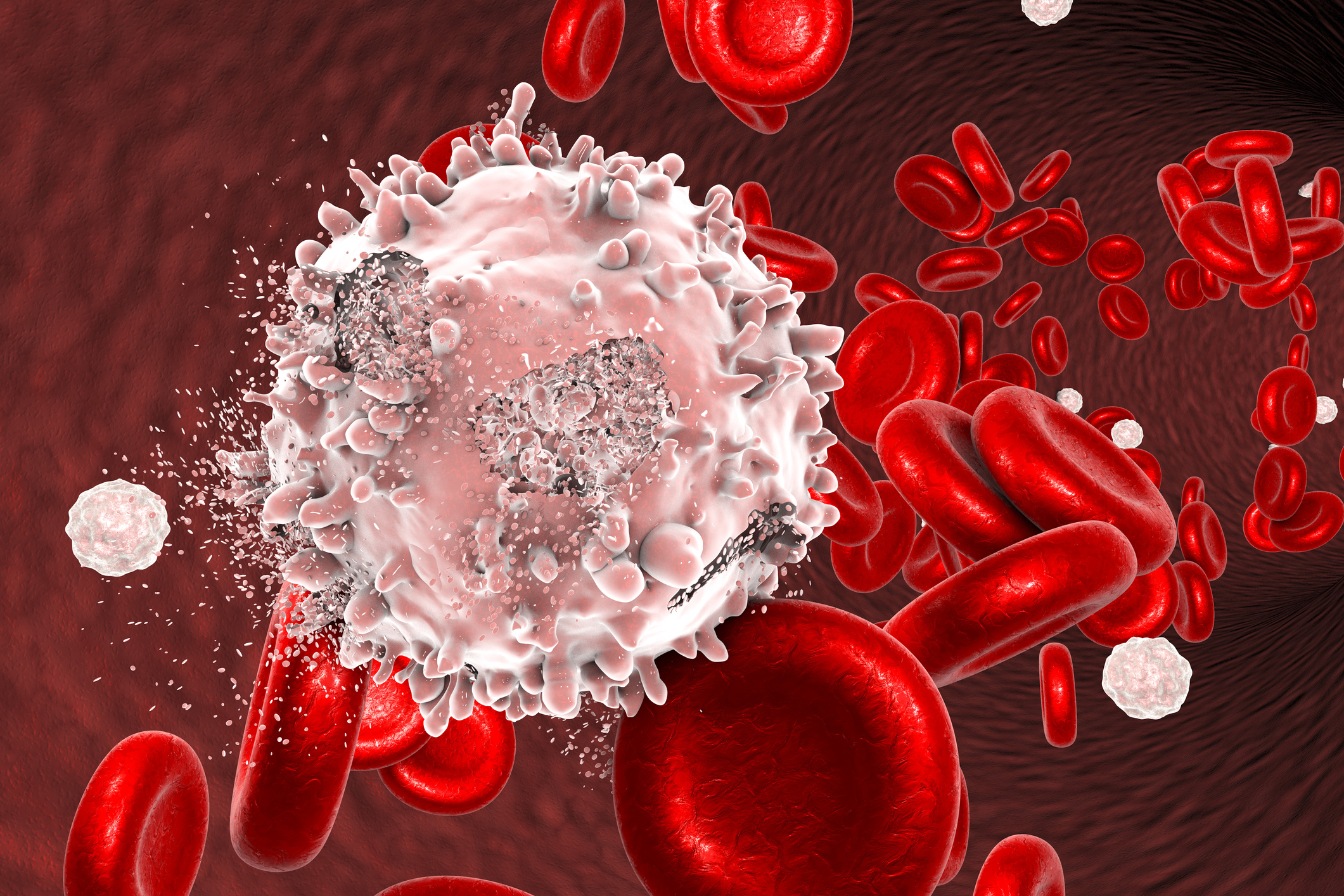
A BC-based team of TFRI-funded researchers has discovered that CD33, a protein from the sialic acid-binding receptor family that was previously believed to be unique to normal maturing white blood cell precursors and acute myeloid leukemias (AML), is also present on human cord blood stem cells with the highest regenerative ability.
The findings, published in Nature Cell Biology (June 2018), could significantly affect the design of targeted AML therapies, according to Dr. David Knapp (BC Cancer/UBC) and Colin Hammond (PhD candidate, UBC), the study’s two co-first authors.
“This finding suggests a potentially serious complication with some current anti-AML treatments that aim to kill all cells expressing CD33,” said Dr. Connie Eaves (BC Cancer/UBC) who led the team study funded by a Terry Fox New Frontiers Program Project Grant.
This new discovery provides a possible explanation of why some trials that have used CD33 as a potential target for AML therapies have shown specific toxicities expected from a loss of normal stem cells, according to the Eaves’ group.
Their investigation also revealed previously unknown functional and molecular differences between individual human blood stem cells. The study also sets the ground work for identifying shared features that could be critical to the high regenerative ability unique to these rare cells.
“This paper presents the first description of associated molecular and biological properties of individual human blood stem cells and has made the detailed results available in a permanently accessible form for other investigators to consult and use,” Hammond said. “These findings could thus be a major aid to the development of better protocols for expanding human blood stem cells in the laboratory, and therefore contribute to an improved availability of donor cells useful for clinical transplants.”
Study
Single-cell analysis identifies a CD33+ subset of human cord blood cells with high regenerative potential
Authors
David J. H. F. Knapp, Colin A. Hammond, Tony Hui, Marijn T. J. van Loenhout, Fangwu Wang, Nima Aghaeepour, Paul H. Miller, Michelle Moksa, Gabrielle M. Rabu, Philip A. Beer, Davide Pellacani, R. Keith Humphries, Carl Hansen, Martin Hirst and Connie J. Eaves.
Funding
This work was supported by a TFRI New Frontiers Program Project Grant in Exploiting Pathogenic Mechanisms in Acute Leukemia for Clinical Translation.