For nearly two decades, researchers studying prostate cancers have known that the loss of PTEN, a tumour-suppressing gene, plays an important role in disease progression. But until now, tying PTEN loss to a specific prognosis – or an appropriate clinical decision – has been nearly impossible.
A new study by researchers from Queen’s University in Kingston, ON may help change this. In a paper published in the Journal of the National Cancer Institute (March 2020), the team identified the specific threshold at which PTEN loss becomes clinically significant, positioning it as a potential tool that could help guide what kind of treatment a patient receives after a prostatectomy.
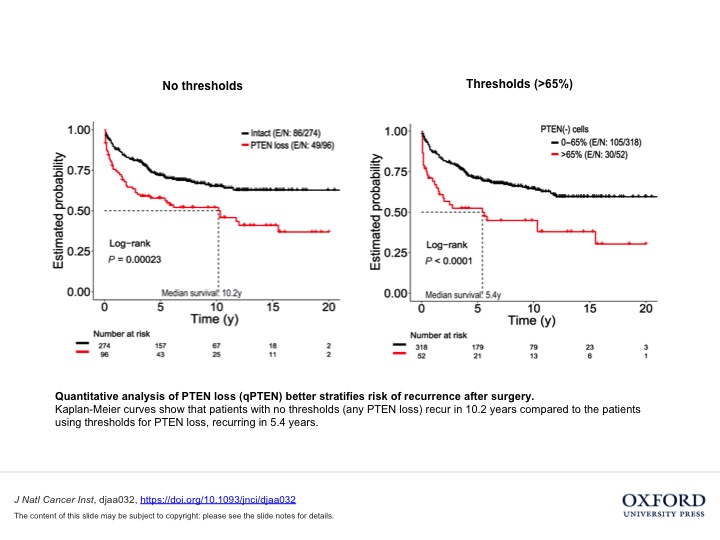
“We discovered that there is a specific threshold below which PTEN loss has no clinical relevance. Essentially, if 65 per cent or less of a patient’s cells have PTEN loss, those patients won’t behave differently than patients with no PTEN loss,” said Dr. Tamara Jamaspishvili, the paper’s first author and holder of a TFRI-funded molecular pathology fellowship. “However, for certain types of patients above that threshold, relapse time is twice as fast as it would be otherwise, which suggests that they might benefit from adjuvant treatments after surgery.”
To reach this conclusion, the team used tissue microarrays from prostate cancer patients collected through the TFRI-funded Canadian Prostate Cancer Biomarker Network. Digital image analysis was used to quantify the amount of PTEN loss in each sample and advanced statistics were deployed to find a threshold at which this loss had clinical relevance. The findings were then validated with samples from different centres.
This novel approach will help standardize PTEN testing, while also providing a roadmap that can be applied to other pathology tests that are still highly subjective.
Moving forward, the team is hoping to further validate this novel quantitative method of biomarker testing on diagnostic biopsy samples that will be collected through both retrospective and prospective clinical studies. They are also working to automate PTEN digital pathology analysis using deep learning approaches, which could fill the gaps between research and clinical practice and make patient management more targeted and personalized.
“As a surgical pathologist in charge of diagnosing prostate cancer and conducting routine testing that guides treatment, I’m interested in finding molecular tests that can actually guide clinical decisions, because there aren’t many available yet,” said research team leader Dr. David Berman, a surgical pathologist at Queen’s University and the director of the Queen’s Cancer Research Institute. “We hope that once this is validated, measuring PTEN loss right after surgery will give us a clear indication of whether a patient should be monitored for relapse or proceed to adjuvant radiation.”
Study
Risk Stratification of Prostate Cancer Through Quantitative Assessment of PTEN Loss (qPTEN)
Authors
Tamara Jamaspishvili, Palak G. Patel, PhD, Yi Niu, Thiago Vidotto, Isabelle Caven, Rachel Livergant, Winnie Fu, Atsunari Kawashima, Nathan How, John B. Okello, Liana B. Guedes, Veronique Ouellet, Clarissa Picanço, Madhuri Koti, Rodolfo B. Reis, Fred Saad, MD, Anne-Marie Mes-Masson, Tamara L. Lotan, Jeremy A. Squire, Yingwei P. Peng, D. Robert Siemens, David M. Berman
Funding
This study was partially funded by a Terry Fox Translational Research Program Grant to the Canadian Prostate Cancer Biomarker Network and the Terry Fox Research Institute Cancer Research Training Program for Clinician-Scientists in Molecular Oncologic Pathology
COVER IMAGE CREDIT: Nephron / CC BY-SA (https://creativecommons.org/licenses/by-sa/3.0)